Big data Machine learning Data visualization
Fill the form to download the case study
Client acquired the closest pharmacy benefit management (PBM) competitor, to align the rules between the client’s PBM and the acquired PBM solution is required to execute claims of recent three months then Identify positives, false positives, and mismatches.
e-Zest’s solution approach was to develop the technical components of claims comparison solution to create claim request files, process response files. The strategy was to compare data, apply business rules and algorithms, develop a dashboard for analysis and verification using big data technology stack. The provision was there to extend it to do parallel-run for claim prediction, anomaly detection, fraud detection, and other use cases.
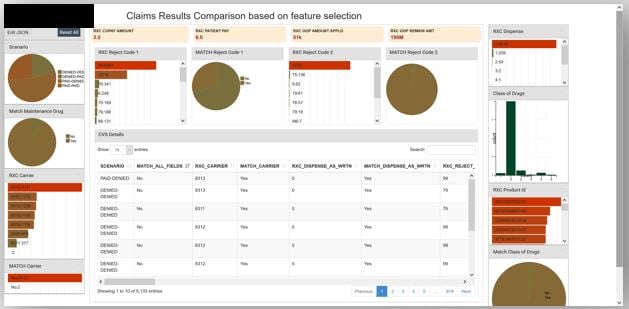
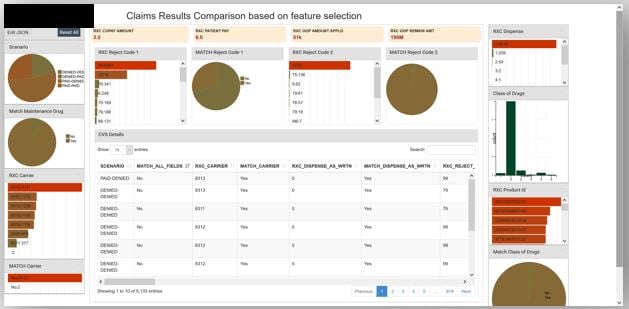
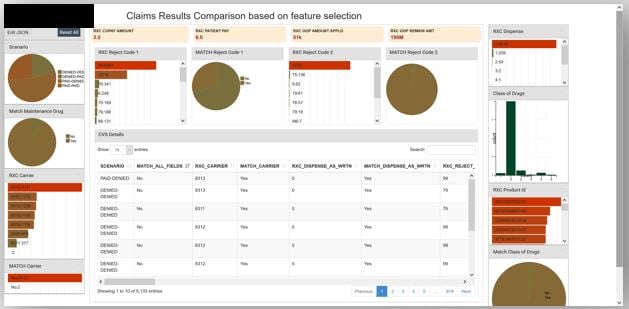
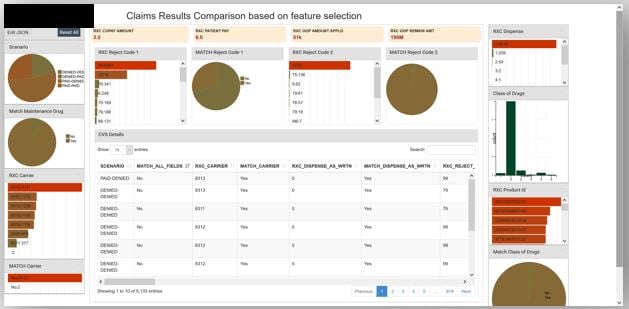
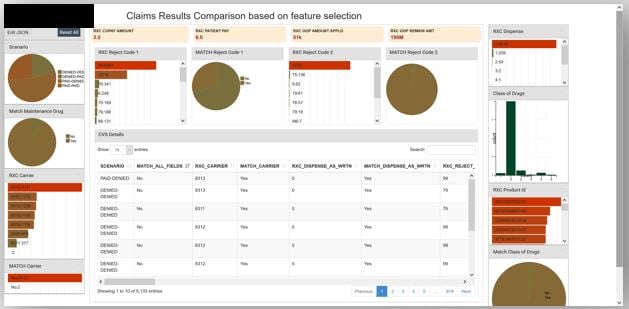
Efforts had resulted in an end to end visualization-based solution which can display records of false positives as well as mismatches. The algorithm behind data comparison became mature with every passing day on processing millions of records and resulted in deeper refinements in the analysis of claims and certifications to align rules across both the PBMs, the solution was developed with NCPDP D.0, HIPPA, CMS, PPHI and IT compliance.
e-Zest is a leading digital innovation partner for enterprises and technology companies that utilizes emerging technologies for creating engaging customers experiences. Being a customer-focused and technology-driven company, it always helps clients in crafting holistic business value for their software development efforts. It offers software development and consulting services for cloud computing, enterprise mobility, big data and analytics, user experience and digital commerce.